If you have celiac disease and IBS, you aren't alone. I'm right there with you!
This post may contain affiliate links. Please see my disclosure page for more information. Thanks!

Ever since I was a teen, I've had a nervous stomach. Now as an adult, I have Irritable Bowel Syndrome -Diarrhea Type (IBS-D).
It's tough to have one digestive ailment, like celiac. But after 12 years of living gluten-free, I'm very proficient at staying safe. Unfortunately with IBS, stress is the culprit. And that's a little bit more challenging to avoid 100% of the time!
As I've learned more about IBS and my symptoms, I can now recognize when I'm having an IBS flare or when I've been exposed to gluten. I also know my triggers and how to help manage my stress to avoid symptoms.
To be honest, I find IBS more debilitating than celiac. It's affected my health a lot more than celiac disease has as an adult.
Here's how I deal with both of these digestive ailments and eight tips for you if you also have celiac disease and IBS.
Disclaimer: I am not a medical professional, doctor, or healthcare provider. This post is not meant to diagnose, cure, or treat illness. I am simply sharing the information and resources that have helped me navigate having both celiac disease and Irritable Bowel Syndrome. If you are struggling with symptoms, please speak to your doctor. I hope you feel better soon.
Celiac & IBS: 8 Tips For How I Handle Both
- Celiac & IBS: 8 Tips For How I Handle Both
- What The Research Says
- My Top Tips For Navigating Celiac & IBS
- Have a solid support system and medical care team.
- Recognize how gluten exposure compares to an IBS flare.
- Manage your stress. No, seriously.
- Know your trigger foods.
- Keep emergency supplies with you at all times.
- Don't overdo it with gluten-free menus!
- Meditation & Journaling
- It's not always what you eat, but HOW you eat.
- Final Thoughts: Celiac Disease & IBS
What The Research Says
Before we begin, I want to reiterate that I am not a doctor or medical professional. I rely on what the research says about IBS, my doctor's advice, and knowing my own symptoms.
There are some interesting data points about celiac disease and IBS and how they are related. While celiac disease is often misdiagnosed as IBS (which unfortunately happens a lot), the number of people with IBS is higher if you already have celiac. According to Beyond Celiac, "the prevalence of celiac disease in people who also have IBS is 4 times greater than in the general population".
Whoop there it is.
Additionally, according to the Celiac Disease Foundation, "at least 20% of individuals with celiac disease continue to have symptoms on a gluten-free diet". That's exactly what was happening to me post-celiac diagnosis and post-SIBO treatment. Quickly I started to realize that stress was contributing a lot to my stomach problems. It took many years to finally be able to pinpoint what strategies worked well for me to prevent flares.
My Top Tips For Navigating Celiac & IBS
Have a solid support system and medical care team.

One of the most important things you can have in your life is a solid support system and medical care team.
Dylan is my champion. He eats gluten-free when he doesn't need to, makes me tea when my stomach is feeling off, and is willing to eat at home a lot when I'm having a flare-up or gluten reaction. I'm very lucky to have him. Additionally, I have very supportive and loving parents who were quick to get me the proper care I needed during my initial celiac diagnosis as a teen and continue to look out for me as an adult. Thank you, Mom and Dad.
Over the years I've had some doctors and medical professionals not take my problems seriously. I had a doctor who told me I would have to take Imodium every day for the rest of my life (when I actually had SIBO that wasn't treated properly). I also had a nutritionist tell me the reason I was having stomach problems was due to an ingredient in granola bars and that I ate too much salad.
Um, no. Both of these people did not help me. AT ALL. In fact, they only made me more stressed out.
If you find your doctor or medical care team is not listening to you, it's okay to see someone else. You deserve to be listened to with respect and taken seriously. Thankfully, my primary care physician (who I've been going to since 2012) is an absolute gem, and my new GI doctor is much better. But it took some trial and error to find a GI doctor who took my needs seriously.
Recognize how gluten exposure compares to an IBS flare.
This can be hard to do. But with time, you may be able to tell the difference between an IBS flare and a gluten exposure. Tracking your symptoms with a food journal can help.
For me, gluten exposures last for up to 48 hours. I have major brain fog and feel "off" after I've been exposed. But an IBS attack is quick and done. Once it's over, I feel a thousand times better and have no lasting symptoms.
It may be different for you. Talk to your doctor or medical team for help in distinguishing them.
And if you can identify the differences between the two, it may help prevent you from unnecessary panic or stress. Sometimes a stomachache might just be stress-related, and not that you've unintentionally glutened yourself.
Manage your stress. No, seriously.

Stress is the #1 reason my stomach acts up.
Even when I don't think I'm stressed, or nervous, or anxious, my gut-brain connection says differently.
This can also happen to me when I'm excited about something too!
Specific situations where this has happened to me & I had an IBS attack:
-the day before school would start, as a student, or as a teacher.
-the day of a big concert in college (I played violin on a scholarship for 4 years)
-after an emotional or traumatic event, like the death of a loved one
-the days leading up to an exciting event, like a wedding that I'm a part of
The only time I was able to prevent an IBS flare was my wedding day. I took Imodium for a few days prior just in case. I may have been constipated for a day or two after, but it was better than the alternative of sh*tting my pants down the aisle to Dylan.
Ways I practice de-stressing include:
-turning off my phone and keeping away from social media
-going outside in nature, preferably a hike
-reading a book (a real book, not an electronic one)
-taking a hot bath or shower
-talking about my feelings to someone or writing them in my journal
-SLEEP.
Know your trigger foods.

For me, they are sugar, dairy, and butter. I used to have issues with onions and garlic while dealing with SIBO (Small Intestine Bacterial Overgrowth), but they are no longer a problem.
I'm slightly lactose intolerant, and Lactaid definitely helps me digest dairy. But if I go overboard, it ends up ugly.
Keeping a food journal and tracking my symptoms has helped with this a lot. While it can be annoying to constantly write down what you eat/drink, it honestly helps. It can also give you more information and sometimes control over your symptoms if you know exactly what will set them off (sometimes, but not always. Sometimes it doesn't matter what you eat and you can have a flare anyway.)
Keep emergency supplies with you at all times.
I used to operate on the mindset of "Nah, I won't need it." But after too many late-night trips to CVS, I've determined it's much better to be prepared with the things I need in case of an emergency.
For me, these include:
-Lactaid Pills
-GasX
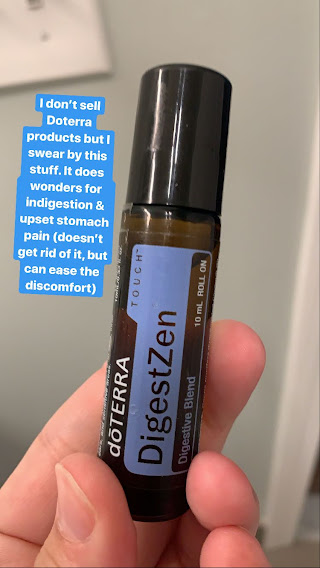
-Peppermint Essential Oil Roll-On From DoTerra
-PooPurri
-Comfy Sweatpants & leggings that are bloat-friendly
These work for me. Decide whatever you know gives you relief and check with your doctor about what can help.
Don't overdo it with gluten-free menus!

Do you know that feeling you get when you go to a restaurant where they have dedicated fryers & really strong allergen protocols?
It's like your brain can only think of one thing.
FRENCH FRIES. FRIED THIS. FRIED THAT. FRIED EVERYTHING.
Dedicated fryers are like the holy grail for gluten-free people. And when we see that as an option, we want in!
Deprived so often of foods we cannot have, when we can finally have them safely, we go overboard.
But then, when our stomachs hurt later, we panic.
Was that gluten-free?
Did I not self-advocate enough?
Why does my stomach feel so awful?
And then that stress can only compound the problem!
More often than not, your food WAS safe, but you stressed yourself out into thinking it wasn't. When really, it was just that you went a little overboard with the fried foods.
Take it easy when it comes to gluten-free menus. It's of course okay to indulge and you deserve to enjoy all of those foods like everyone else. But if you go crazy, your stomach will tell you.
Meditation & Journaling
Meditation has been a HUGE help for me in managing my day-to-day stress. It might sound totally hipster, but honestly, it helps. I use the app/website Calm for meditation. This is not sponsored but a heartfelt recommendation and I use it DAILY. I meditate during the day or at night before bed. I use it for tracking my thoughts, resetting my focus, deep breathing, and falling asleep. It's wonderful.
I also journal my thoughts and feelings. This is especially helpful if you feel like you can't voice the things you want to say out loud. But getting it out is so important and can be a weight off of your shoulders for sure.
Additionally, retraining your brain in times of stress through hypnotherapy is one of the actual treatments for IBS. If you've read anything about the brain-gut connection, you know how crucial this is. Check out the app Nerva for ways you can do this right on your phone.
It's not always what you eat, but HOW you eat.
When I was teaching, I needed a lot of food to keep me going. I would use up a lot of energy managing students, talking, and walking around the classroom, and around the building. It was a good amount of work!
But the one thing that never really sat well with me was, well...breakfast!
Even though I always wake up starving, (I have a fast metabolism), I would be eating breakfast as early as 6:00 or 6:30 AM, right after waking up. And my body did NOT like that.
I would have a lot of gas in the mornings and feel really bloated until lunch.
But once I started teaching from home during the pandemic, I wasn't getting up as early, which meant I wasn't eating as early, but just sipping tea for the first few hours of the day.
And VOILA!
My morning stomach problems were gone. I still had to use the bathroom in the morning (because, um, duh), but it was normal and without issue. No more gas or bloating. Now, I follow the same procedures and it helps so much.
Hallelujah!
I've also noticed this is applicable to eating other meals. If I eat too fast, I can end up with symptoms. Eating slowly, chewing food thoroughly, and sitting down for meals all help. With IBS, it can often be not just what you're eating, but the way you're eating that can have an impact on your symptoms.
Final Thoughts: Celiac Disease & IBS

Having both of these digestive troubles can be HARD. But when I have a flare-up or a gluten reaction, I always remind myself to be kind to my body, and not beat myself up. Adding additional stress doesn't help. It's best to forgive, rest, and move on.
If you are struggling with both celiac disease and IBS, I'm sending you virtual hugs as you read this. I'm right there with you and hope you can find relief.
If you are struggling with stomach problems relating to celiac disease or IBS, please speak to a medical professional. Here are some resources that can help. Also, go follow my friend Christine @myibslife on Instagram for a laugh about living with IBS, and checkout Erin Judge, RDN a dietitian who specializes in IBS on Instagram.
How do you manage both celiac disease and IBS?
Let me know in the comments below.



Dan says
Can’t tell you how relatable this is. It’s been so hard for people to say “well you wound yourself too tight that’s why you have an upset stomach” and I know my anxiety is a big part of my IBS.
With that, I decided to try CBD Oil to help with calming. So many doctors want me on antidepressants but I don’t want to live my life like that: there’s no shame in taking medications but for me I don’t want to rely on them.
Thank you for sharing your experience
Jennifer Fitzpatrick says
Thank you so much Dan for commenting. Holding space for you and the challenges of IBS. It isn't easy. Appreciate you following along.
-Jen
Karen says
Wow. So glad I found this. Yes, I relate. I have heaps of food intolerances due to IBS and celiac disease as well. I have been diagnosed with both for 3 years and suspected that I was not alone. It's just a relief to know this is true. And like you I really feel it is much harder to deal with the ibs than being gluten free. Thanks for the tips. I already do most of these but it's great to know I am on the right track. And I did get 1 new idea from your list. Thanks so much. From Australia 🌏
Jennifer Fitzpatrick says
Karen, hello! Thank you so much for reading this post and for sharing your story. Holding space for you dealing with both of these challenges too. I completely understand - the stress piece can be so debilitating with IBS, and I'm glad my list gave you some new tips. Sending hugs from the USA to you in Australia!
Graham says
Hey Jennifer,
I just wanted to say “thank you”!!!
It has been quite a bumpy road for me following my Celiac diagnosis, and more recently IBS.
Reading your post gives me hope that it will be manageable one day.
I hope to one day find the support system that you have found, as I believe that will help. Hard when the healthcare system has little knowledge of these diseases.
Find it difficult navigating between the two, don’t know what there is left to eat.
Keep up the good work, you have no idea the hope you are giving to others.
Jennifer Fitzpatrick says
Thank you Graham for this lovely comment - it has truly made my day as I'm dealing with an IBS attack right now! So thank you for taking the time to leave a comment. Sending good thoughts and healing your way as you navigate these tricky diagnoses and that you have a solid support system that listens to you. Take care!
Jessica says
Thank you so much for sharing. It really helps to know I’m not alone. I’m 20 years old and was diagnosed with Celiac at 8 years old. I was healthy for a few years on a Paleo diet but got sick again for the past 2 years (acid reflux, constipation, gas, bloating) and only discovered this summer (on my own) that IBS is the problem. I’m doing so much better on a low Fodmap diet but it’s so easy to mess up and I deal with flare ups all the time. I often beat myself up and get really upset but it’s comforting to know I’m not a complete anomaly and that I can eventually learn to manage and stay healthy.
What has been key for me is pre portioning all foods before eating according to the low FODMAP diet (I highly recommend the apps FODMAP A to Z, FODMAP friendly). Watch out for hidden sources of garlic if that’s a problem for you (often on chicken and other meat, dressings, ketchup etc) Also, the Fig app is really helpful for anyone with a restricted diet- you can scan any food product and it tells you if it’s safe to eat and about any potential cross contamination or hidden sources of the foods you’re avoiding. The most important strategies for me have been to really pay attention to my bodies signals, look out for what foods might be causing a problem, and stay patient.
gemma says
Loved reading your journey with Ibs and celiac. Diagnosed with both 4 months ago and really struggling. Cannot gain any weight back!
I feel like everything I eat is still causing issues. And,yes, stress levels through the roof
Jennifer Fitzpatrick says
Sending you the biggest hugs, Gemma! I hope you find relief soon!
Gemma Stotler says
So glad I found your story! I have had stomach issues all my life. Finally diagnosed with Celiac 6 months ago. Also dealing with IBS. Your story was a mirror image of what I am dealing with . And, yes, stress is a major factor. My mornings are the worst. Helps so much to read others are also fighting the battle! Thank you for sharing.
Jennifer Fitzpatrick says
You are NOT alone, Gemma! Sending you big hugs and know that if you need more support I offer that too!
Josie says
Hi I have celiac disease and IBS
Thank you for your story..,it’s very encouraging..
I have had celiac disease for three years and IBS followed..I have had stomach issues all my life but people and I thought it was nerves ..I deal with this everyday even when I don’t eat gluten which I don’t I get these stomach aches
It’s more my IBS that acts up and it czn be so annoying ..I sm 54 years old and also have arthritis and psoriasis
Thank you for listening
Josie
Jennifer Fitzpatrick says
Sending you BIG HUGS Josie! Have you looked into Nerva, the hypnotherapy app? It's one of the treatments for IBS and might be able to help! It's not easy having your anxiety/stress manifest in stomach problems, and I know that firsthand.
Tracey Perry says
I am glad I found this article, I found it very interesting. I have Coeliac's and have been suffering a lot of stomach pain lately. I believe it is down to stress and possibly other triggers, but I am definitely going to start a food diary to see if there are more food types that I am having a reaction too. But I always think the worst. Last week I was in and out of the hospital for 2 days having tests for a suspected appendicitis, it wasn't and the pain disappeared after a few days. Thank you, I needed this to remind me that we have to love our bodies and to be kind to ourselves.
Jennifer Fitzpatrick says
Holding space for you, Tracey! I'm so sorry you've been suffering so much lately with all that pain. Wishing you peace, healing, and lots of self-love on your journey. Thank you for reading.